End of Life and Hospice Care

What is end-of-life care?
Making decisions about end-of-life care is difficult. Along with the roller coaster of emotions and uncertainty, the complexity of the medical options makes it challenging to come to the right decisions for you and your family. The good news is that palliative care and hospice care are widely available and offer the pain and symptom management and end-of-life care that patients and their families need. These services are regulated at the state and national level and are covered by Medicare and other health insurance companies.
What's the difference between palliative care and hospice?
Although both palliative care and hospice care provide the patient with comfort and support, they are not the same.
Palliative care can be provided earlier on in a patient's diagnosis, while they are still aggressively treating a disease. Palliative care is interdisciplinary care that aims to relieve suffering and improve quality of life for patients with advanced illness and their families. It is offered simultaneously with all other appropriate medical treatment.
Hospice care is provided when a patient and physician have determined that they are no longer going to aggressively treat the disease, yet they will aggressively manage pain and other symptoms. The patient's physician and hospice medical director certify that the illness has a prognosis of six months or less. A question that ought to be asked by the physician is "Would this patient survive this disease for one year given its normal course?"
Hospice care focuses on the family members as the primary caregivers, with the help of a skilled interdisciplinary team made up of nurses, physicians, pharmacists, physical therapists, occupational therapists, speech therapists, social workers, spiritual care providers, aides, and many volunteers who provide services such as pet therapy, hand massage, and respite for the caregiver.
Hospice also offers thirteen months of bereavement/grief services to the family or other caregivers. The focus of care is on improving quality of life and asking the patient what they desire during this last stage of life. These services can be provided in the home, in a hospice residence, or in a skilled nursing facility, assisted living center, or group home.
The central issue: Pain management
"Control of pain is really the heart of terminal care. People do not fear death so
much as they fear unrelieved pain and being alone with their suffering."
~ Deborah Whiting Little, The Family Handbook of Hospice Care
Many terminally ill patients experience physical pain or discomfort. Physical pain is our body's internal regulatory system alerting us that there is something wrong. Thus pain can be an important indicator of issues that need to be addressed. Physical pain can be acute (sudden) or chronic (long-lasting), and both need to be addressed.
The fear of pain may occupy much of a patient's thoughts. It can also bring about emotional stress and tension, which can prevent pain medications from working properly. The focus is always to offer optimal pain control and to reassure the patient that their pain will be managed. The goal of pain management is to relieve and prevent the pain from recurring.
To manage pain, it is important to assess it. Healthcare professionals and family members can ask a patient the following questions:
- Where is the pain?
- On a scale of zero to ten, with ten being excruciating, how intense is it?
- It is continuous or does it come and go?
- Can you describe it? Does it throb or ache?
- What seems to help it? What makes it worse?
(The Family Handbook of Hospice Care)
With this information, experienced healthcare professionals can determine a pain management strategy. Pain will change over time, so it is important to assess and adjust the plan regularly. Medications and other interventions also can be added/increased and changed to respond to these assessments.
In addition to physical pain, a patient might experience emotional, psychosocial, financial, or spiritual pain. Hospice care includes social workers, spiritual care providers, and other professionals to help patients and families talk about their fears, anger, and grief and alleviate emotional and spiritual pain.
When is hospice appropriate?
As mentioned above, hospice care is typically appropriate when a physician or team of healthcare professionals agrees that a patient's life expectancy is six months or less and the patient is not responding to curative treatment. There are diagnostic tools that can help clinicians determine a patient's prognosis associated with different diseases and conditions.
A helpful question that patients and families can ask the physician is: "Would this patient survive a year with the disease as it is now?" The patient and his family members ultimately make the decision whether or not to begin hospice.
Hospice may be considered for the more advanced stages of following diagnoses, among other conditions:
- Cancer
- Heart disease
- AIDS
- Pulmonary disease
- Neurological conditions
- Chronic diseases
- Alzheimer's disease
- Amyotrophic lateral sclerosis (ALS)
- Severe stroke
- Renal failure
What conventional services does hospice offer?
Typically, patients who are receiving hospice care receive the following:
- Visits from nurses who have been educated in pain and symptom management. There is also a nurseline, which patients and families can call 24 hours a day with any questions.
- Assistance with bathing and personal needs from hospice aides
- Medications and other medical supplies needed to reduce pain and discomfort related to the terminal diagnosis
- Counseling and bereavement support for the patient and family members, provided by social workers or counselors
- Visits from spiritual care providers, as desired
- Trained volunteers to help the patient and family with various tasks
- Speech, occupational, and/or physical therapy, as needed. These therapists can help identify a patient's skill level regarding communication, movement, strength, and range of motion, and provide tips about how to best communicate with your loved one or how and when to assist them with daily needs.
How to find hospice care in your area
To find a hospice facility or program, talk to your or your loved one's physician or other hospital or clinic staff member. Contact your insurance company to ask which programs or facilities are approved under your policy.
There are more than 5,300 hospice programs in the United States. See the resources in the references below for more information. You can search for hospice providers by location using the National Hospice & Palliative Care Organization's website.
What can you do for your loved one?
Participate in family meetings with your loved one's medical team and be sure to request a consultation with palliative or hospice care when you and your family feel it's the right time. Discussing your loved one's goals and having conversations about advanced care planning are extremely important.
Provide Basic Physical Support
Hospice care uses the family members as the main caregivers with the support of a professional care team, so you will undoubtedly continue to provide basic support, such as preparing meals and helping your loved one eat or drink. As time goes on, this basic support will increase. You may need to help your loved one get changed, bathed, and toileted. You may have a role in helping them track and take medications. Use the care team as a resource to find out what you can do to best help and keep your loved one comfortable. Because these changes will occur suddenly or incrementally over weeks and months, it is important to enlist hospice assistance early. Hospice is not a loss of hope; rather, it adds life to days. Most of those who do receive hospice care report that they wished they would have started hospice services earlier.
Offer Comfort
You can do much of this yourself at home or in residence. For example, you could learn how to give a hand massage with lotion to provide comfort to your loved one. Or you could find music they like that is soothing. You can offer to give a manicure or read aloud.
Help with Lifetime Planning
Another way you can help your loved one is by helping plan for the future by getting all financial, personal, health, legal, and other information in order. Although it is not easy to broach these topics, it is important to help your loved one make these arrangements so he or she can feel closure and remain calm through the rest of his days. This planning includes bank accounts, wills, living trusts, power of attorney, healthcare directives, and funeral arrangements.
What integrative therapies might be helpful?
Integrative therapies can complement other therapies and allow the care team to take a holistic approach to you or your loved one's hospice care. These therapies can help provide comfort and improve quality of life during a patient's final months or days. Your hospice nurse should be able to tell you about programs or therapies available to you and your loved one.
Some therapies for patients and family members to consider are discussed below.
- Massage Therapy, reflexology, Healing Touch, and Reiki are hands-on therapies that provide comfort and relieve symptoms through the use of physical manipulation of muscles or through energy healing. They may also help the patient deal with pain, anxiety, or sleeplessness. A recent study of more than 300 hospice patients with cancer showed that massage therapy may provide pain relief and improve patients' moods, according to the National Center for Complementary and Alternative Medicine.
- Aromatherapy can provide many benefits to patients and family members. Some essential oils may help alleviate nausea or fatigue, while others may help with anxiety and depression.
- Music Therapy - Music can be soothing, relaxing, nurturing, energizing, or comforting. It may provide the following benefits:
- Reduce anxiety and stress
- Promote relaxation
- Strengthen family bonds
- Trigger memories or initiate reflection on one's life
- Improve alertness
- Reduce one's perception of pain or nausea
- Create joyful experiences
- Art Therapy - Art therapy can help individuals explore their emotions through the use of various art mediums. It provides an outlet for creative, non-verbal expression of their feelings.
- Guided Imagery, meditation, or other relaxation techniques can help patients and family members reduce anxiety and put their minds and bodies at ease. These techniques may be done individually or with the guidance of a trained instructor or counselor.
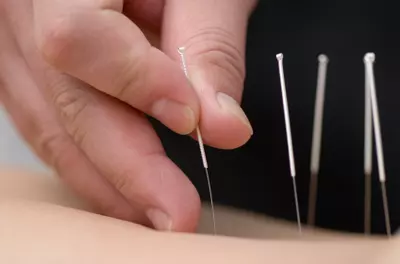
- Acupuncture or acupressure may be used to help reduce pain and nausea. Some patients who have had an ischemic stroke (a stroke caused by clotting, not a hemorrhage) also find it to be beneficial, as it promotes relaxation. The American Academy of Medical Acupuncture asserts that acupuncture can open up blood vessels to help blood flow and decrease the risk of clotting.
- Heat or cold therapy
What to expect In the dying process
"When someone dies, it is important that those close to him participate in the
process; it will help them in their grief, and it will help them face their own death
more easily."
~Elizabeth Kubler-Ross, The Family Handbook of Hospice Care
As death draws near, it is normal for your loved one to experience anxiety. It is helpful to reassure your loved one that you are there in support, and that although you will miss them, it is okay to let go.
There are certain emotional and physical changes that people typically go through.
Emotional changes may include:
- Withdrawal or shutting out external stimuli, such as television or other people. The patient may seem to sleep more frequently. This is normal.
- Extreme anxiety or restlessness. This may include fidgeting or making repetitive motions with one's hands. You may help your loved one by distracting them with something they love, such as music, or by talking with a nurse about ways to reduce anxiety.
- Confusion or disorientation. Your loved one may get confused about where they are, what day it is, or even who you are. You can help them by gently introducing yourself and giving them reminders about where they are and what they are doing.
- Hallucinations. Your loved one may experience hallucinations, which can be a result of decreased oxygen in the blood.
Physical changes may include:
- Weakness or a loss of sensation
- Skin color changes. Sometimes the skin turns a darker color on the underside of the body, and fingernails and toenails turn a pale blue color.
- Temperature fluctuations
- Muscle twitches
- Changes in breathing patterns. If your loved one breathes through their mouth consistently, they may get dry lips and mouth. You can help by applying chapstick and offering them ice chips, water through a straw, or even a damp washcloth. The breathing rhythm may also alternate between shallow and deep, fast and slow. As the breath slows there may be longer periods between any breath, which are known as "periods of apnea."
- Decreased ability to cough or swallow oral secretions, such as saliva and mucous. This may result in a gurgly sound heard during breathing. You may help by elevating your loved one's head.
- Decreased blood pressure
- Hearing is the last sense to leave, so assume your loved one can hear you even in the final stages.
As death draws near, the signs mentioned above may worsen. Your loved one may experience a burst of energy, during which he might even want to talk to loved ones or eat a meal. Sometimes, people are conscious for a long time, and death comes suddenly. Other times, people may be unconscious and slowly slip away.
Coping with grief
Coping with the death of a loved one can be overwhelming. After the passing of your loved one, bereavement services are available for family members for one year (and sometimes more). These services can help you cope with your grief, as well as guide you as you take care of practical matters.
There is neither a standard amount of time that you should grieve nor a particular way in which you should grieve. Grief is unique to everyone. However, there tend to be some phases of grief that people may experience at different times during their own grieving process. These phases include:
- Shock and denial
- Longing for connection to your loved one
- Despair and disorientation
- Adapting and acceptance
During these phases, you may experience emotional and physical stress. Physically, you may lose your appetite or struggle to fall asleep at night. Or you might experience tension in your stomach or another part of your body. Emotionally, you may experience depression or loneliness. Some people may not experience stress after a loved one dies. This is also normal.
No matter how you express your grief, it is important to do so. This can come out in crying, talking with friends and family, writing in a journal, talking with a bereavement counselor, praying, or any other activity that allows you to process your loved one's death. Bereavement counselors recommend grieving, but not allowing the grief to overcome you or cause you to be paralyzed by it.
The staff at Fairview Hospice educate with the following: "Grief is a natural response to loss. Grief is experienced physically, emotionally, and spiritually. Grief is a process that takes time and attention in order to heal. Grief is as unique to you as a thumbprint."
Read more about managing stress.
Resources
Important Phone Numbers
Hospicelink - directory of hospice and palliative care programs in the U.S. 1-800-331-1620
Minnesota Network for Hospice and Palliative Care 651-659-0423
National Hospice and Palliative Care Organization 703-837-1500
Fairview Hospice 612-728-2455