Back Pain

What is low back pain?
Pain in the low back (waistline or below) is a very common problem and affects 80 percent of Americans at some time in their lives. Back pain is one of the most frequent reasons people seek medical care.
It is important to remember that back pain is a symptom. Common cause of back pain include nerve and muscular problems, degenerative disc disease, and arthritis. However, pain arising from other organs may be felt in the back. Other medical conditions, such as appendicitis, kidney diseases, pelvic infections, and ovarian disorders, among others, can cause low back pain.
Most of the time, back pain is relatively minor, and 80 percent of episodes of acute low back pain will resolve within six weeks, regardless of whether you seek treatment or not. However, the following symptoms and warning signs may suggest a more serious condition and should be evaluated by a professional.
Seek medical attention if the pain:
- Extends down your leg
- Increases when you lift your knee to your chest or bend over
- Follows a recent fall or trauma
- Lasts more than three weeks
- Becomes worse when you rest, wakes you up at night, or is associated with a fever
- Is associated with bladder or bowel problems
- Is associated with numbness or weakness in your legs
What are the conventional treatments for low back pain?
The most important aspect of back pain is how it impacts your ability to function in your daily life. So although it's important to reduce pain, the emphasis of the treatment isn't only on eliminating the pain, but on improving your ability to function as much as possible in your usual activities.
Treatment options include a variety of conservative approaches, such as medications, exercise and physical therapy, and counseling, or they include more aggressive approaches, such as surgery.
1. Medications: The choice of medication depends on whether the pain is muscle and bone pain, nerve pain, or a mixture of both.
For muscle and bone pain, the general categories of medications used include:
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen
- Narcotic medications or opioids such as codeine or hydrocodone. These do not treat the underlying cause, but rather mask the sensation of pain
- Muscle relaxants, such Flexeril or Soma. The U.S. Food and Drug Administration (FDA) does not recommend the long-term use of muscle relaxants because they are not effective in actual muscle relaxation after two weeks of use.
For nerve pain, some medications that are not normally labeled as pain relievers (but because of their properties, they may help the body fight pain) might be helpful. These medications, which help the body re-program the messages involved in relaying the pain signals, include:
- Tricyclic antidepressants
- Anticonvulsants
- Selective serotonin reuptake inhibitors (SSRI) antidepressants, such as fluoxetine and paroxetine
- Selective norepinephrine reuptake inhibitors (SNRI) antidepressants, such as effexor and cymbalta
Steroid medications, such as Prednisone and Medrol, can be useful in easing pain and acute flare-ups in inflammation. However, they must be used with extreme caution, especially if they are used for longer a week.
2. Cold or heat therapy: Using cold and heat therapy may relieve pain and muscle tension in the initial days after back pain begins. Cold or ice applied to your back can reduce inflammation and swelling by constricting blood vessels. The cold also acts to slow nerve impulses and make it less likely that your muscles will contract, in this way reducing pain. Some studies show that heat is an effective approach for acute nonspecific back pain.
3. Electrical stimulation: Transcutaneous electrical nerve stimulation (TENS) can decrease pain by delivering a tiny electrical current to key points on a nerve pathway. The current, delivered through electrodes taped to your skin, isn't painful or harmful.
4. Cognitive behavior therapy: This type of talk therapy combines attempts to identify unhealthy, negative beliefs and behaviors and replace them with healthy, positive ones. It's based on the idea that your own thoughts determine how you behave. This therapy may have a role in the case of chronic low back pain for which no specific physical cause is evident.
5. Multidisciplinary treatment programs: A multidisciplinary approach to treating low back pain may include a combination of exercise, physical therapy, education, cognitive behavior therapy, vocational counseling, and other strategies.
6. Injections: Anesthetics, steroids, or narcotics into soft tissues, joints, and other areas can be injected in and around your spine. The purpose of such injections is to block nerve conduction, relieving pain.
7. Surgery: There are several different types of back surgery, depending on the underlying problem causing the back pain:
- Diskectomy removes the herniated portion of a disk to relieve pressure on a nerve.
- Laminectomy removes the lamina (bony structure) that overlays the spinal canal to relieve nerve pressure caused by spinal stenosis.
- Spinal fusion permanently connects two or more bones in your spine.
- Intradiscal electrothermal therapy (IDET) involves inserting a heated needle through a catheter into the disk, which thickens and seals the disk wall.
- Vertebroplasty injects bone cement into compressed vertebrae.
Consider all your options, and consider getting a second opinion from a qualified spine specialist before you agree to back surgery.
What lifestyle changes are recommended for low back pain?
Exercise and Physical Therapy
Physical activity plays a strong role in recovering from back pain and particularly in helping to prevent future pain and loss of function. An exercise program can include any or all of the following components: flexing, stretching, endurance training, strength building, and aerobic activity. There is no one-size-fits-all approach. Exercise programs are individualized because people have different levels of pain and differing injuries that caused the pain initially.
Improving the strength, endurance, and function of your back helps minimize the chance of recurrence of back pain. One study showed that people who exercised after an initial episode of acute low back pain were less likely to experience a recurrence of that pain than people who did not exercise after the initial pain.
Any mild discomfort that you may feel as you begin an exercise program should gradually ease as your muscles become stronger. The key is to start an exercise program at a low level to ensure your comfort and proper technique, and then progress slowly as your symptoms allow. Exercises for specific muscles that stabilize the spine may help reduce the low back pain.
Diet/Weight
Obesity is a leading cause of back pain. Reducing your weight by only 10 percent can make a big difference in decreasing back pain. Extra abdominal fat and weight on the pelvis pulls the body forward and puts strain on your lower back muscles. Although obesity may not be the cause of the pain, it takes the pain to a whole new level. Extra weight throws off your posture and makes it difficult to properly align your body for a good sleep. It requires your back muscles to pick up the slack. Eat a healthy diet to maintain an ideal weight.
What are some integrative therapies and healing practices to consider for low back pain?
Low back pain most often results from a combination of physical, mental, and emotional factors.
Many people suffering from low back pain have started using integrative therapies: in a 2003 NIH survey, 54 percent of individuals with back or neck pain report using these therapies annually. (The survey referred to them as alternative medicine.) An integrative approach works well with low back pain, not only to relieve or eliminate immediate pain, but to reduce long-term recurrence and minimize physical limitations.
Manual therapies
Chiropractic
Back pain is the most common reason that people seek chiropractic care. Studies have shown that after six months, chiropractic manipulation reduces pain and disability to the same level as conventional medical care, but with higher levels of patient satisfaction and no side effects from medications. Manipulation of the lumbar area has very low risks.
Osteopathy
Osteopathic manipulation is distinctly different from chiropractic manipulation. Some studies have found no difference in outcomes between osteopathic manipulative therapy and approaches such as physical therapy, ultrasound, and transcutaneous electrical nerve stimulation (TENS), although those getting osteopathic therapy used less medication then those using the other approaches. Another study has shown that of a group of conventionally "untreatable" patients, 75 percent were returned to full prior functional status with osteopathic manipulative therapy.
Practitioners recommend that you try at least three to four treatments of either chiropractic or osteopathic manipulation before determining whether they are effective for you.
Massage Therapy
Cochrane reviews explore the evidence for and against the effectiveness of treatments in specific circumstances, based on the best available published information. A Cochrane review found thirteen randomized trials on back pain and massage therapy.
This review found that massage was more likely to work when combined with exercises (usually stretching) and education. Massage produced more benefit in pain reduction and return of function than joint mobilization, relaxation, physical therapy, self-care education, or acupuncture alone. Acupressure or pressure point massage techniques appeared to provide more pain relief than classic (Swedish) massage.
Mind-Body Practices and Stress Reduction
Like any chronic pain problem, low back pain has a strong association with psychiatric issues, like depression, substance abuse, stress, and anxiety. An individual's coping skills, attitudes, and other illness behaviors all impact the extent of continuing pain. A systematic review of research on mind-body therapies in low back pain found strong evidence of positive effects of cognitive therapies, progressive muscle relaxation, and other such techniques.
Mindfulness-Based Stress Reduction (MBSR) is a program of meditation and gentle yoga that has been scientifically validated. It is currently used in more than 200 hospitals and medical centers to complement the medical management of chronic pain and stress-related disorders. Research has studied individuals with many different kinds of pain (not just low back pain) and shown dramatic reductions in pain levels and an enhanced ability of individuals to cope with pain that may not go away.
Yoga is a holistic discipline that includes mental, physical, and breathwork practices. One National Institutes of Medicine study of more than 100 people with low back pain compared a 12-week program of yoga to conventional therapeutic exercise or a self-care book for patients with chronic low back pain. The yoga proved more effective in improving function, decreasing the "bothersomeness" of pain and days of restricted activity, improving general health status, and reducing the amount of medication, and the benefits persisted for at least several months.
Psychological and Emotional Practices
One long established mental/emotional program for chronic back pain is from John Sarno, MD, a rehabilitation medicine physician at NYU School of Medicine. He has diagnosed what he terms tension myositis syndrome, or TMS. This is a psychosomatic illness that causes chronic back, neck, and limb pain that is not relieved by standard medical treatments.
His treatment programs have patients complete mind/body processes to learn about the relationship between emotions and physical symptoms, as well as the power of self-awareness. They then resume their physical activities, but avoid manipulation, exercise, acupuncture, and massage. He reports treating more than 10,000 patients and has published four books about back pain throughout the past 25 years. Research studies have not yet been done to validate his work.
Botanicals and Supplements
People often use non-steroidal drugs (NSAIDs) such as ibuprofen, for short-term relief of back pain. For those who wish to avoid, or cannot tolerate, anti-inflammatory pharmaceuticals (ibuprofen, diclofenac, indomethacin, ketoprofen, piroxicam), some naturally occurring substances have anti-inflammatory effects, with much less risk of gastrointestinal distress. As with any medications, these should ideally be used for limited periods of healing, not for indefinite, long-term use.
Typical doses for each botanical are indicated below. However, you should talk with your healthcare provider before adding botanicals to your health regimen and ask about the right dosage for you.
- Curcumin is the active anti-inflammatory agent found in the spice turmeric. A large double-blind study demonstrated that curcumin was as effective as a powerful anti-inflammatory drug in reducing pain, swelling, and stiffness in rheumatoid arthritis patients, and has also been shown to be effective in the treatment of postsurgical inflammation. A 95 percent standardized extract of curcumin derived from turmeric is recommended. The daily dosage to consider is 400 to 600 mg, taken one to three times per day, when not taken in combination with other products. Theoretically, it should not be used with prescription blood thinners, but human clinical trials to evaluate bleeding risk have not been done.
- Bromelain, extracted from plants in the bromeliaceae family (like pineapple) contains anti-inflammatory enzymes that have the proven ability to suppress the inflammation and pain of rheumatoid arthritis and osteoarthritis, sports injuries, and other joint inflammatory conditions. Bromelain also helps to break down fibrin, thereby minimizing local swelling. The usual dosage is 400mg, one to three times per day (a lower dosage can be used as part of a combination anti-inflammatory formulation). Bromelain should not be used with prescription blood thinners.
- Quercetin is a phytochemical found in the skins of apples and red onions that blocks the release of histamine and other inflammatory enzymes at supplemented doses (minimum 100-1500 mg per day). Although human studies are lacking at this time, anecdotal evidence is strong for this application, as is experimental research investigation. There are no known contraindications or drug interactions.
How to use integrative therapies and healing practices in back pain
Many people who suffer from back pain experience either chronic, persistent pain, or chronic pain with occasional episodes of acute pain. Because long term use of oral medications (e.g. NSAIDS, muscle relaxants, pain-killers, or tranquilizers) is not optimally effective and has risks of side-effects and dependence, you should consider alternative strategies.
To help reduce acute aggravations and avoid additional pain, it is important to have a maintenance/prevention plan. This should include a regular exercise program with stretching, strength training, and endurance and aerobic activities. Yoga is a good base activity for many people.
It can also be beneficial to have an on-going relationship with a manual therapist, be it a chiropractor, osteopath, or massage therapist, as regular bodywork can help prevent additional pain.
A regular meditation or relaxation practice can help you cope with pain, as can a self-reflection practice that honestly addresses emotional awareness and health.
Maintaining a healthy weight is an important practice for preventing and maintaining back pain since it decreases the stress on your muscles.
With these behaviors and relationships as a foundation, you should be well positioned to respond to an aggravation or acute flare, should that occur.
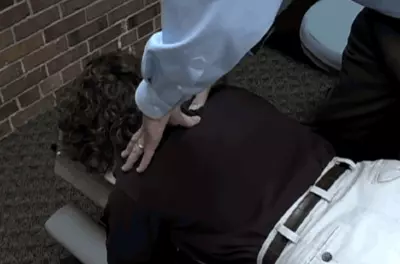
Spine Adjustment Video
Watch this video to see an example of an adult spine adjustment during a chiropractic appointment.
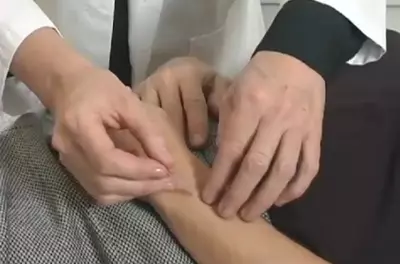
Acupuncture Video
Watch a video of an acupuncture treatment.
Mindfulness and Chronic Pain
Jon Kabat-Zinn describes how mindfulness can help with chronic pain.

Gua Sha Video
Watch this video to see an example of dermal friction treatment.

Cupping Video
Watch this video to see an example of cupping.
Brownstein, A. (1999). Healing Back Pain Naturally: The Mind-Body Program Proven to Work. Pocket Books.
Sarno, J.E. (1991). Healing Back Pain: The Mind-Body Connection. Warner Books.
Dillard, J.N. (2003). The Chronic Pain Solution: Your Personal Path to Pain Relief. Bantam Books.
Weintraub, M.I., Mamtani, R., Micozzi, M.S. (2008). Complementary and Integrative Medicine in Pain Management. Springer Publishing Company.




